Cornea and Keratoconus
The cornea is the transparent, dome-shaped front part of the eye that helps focus light. It acts as an important refractive surface and contributes most of the eye’s focusing power. A healthy cornea is clear, tough, and avascular (free of blood vessels). Its transparency depends on the normal function of all five corneal layers — the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium.
The corneal endothelium, a single layer of non-mitotic cells, plays a key role in maintaining corneal transparency by pumping excess fluid out of the stroma, keeping the cornea slightly dehydrated. When this pump mechanism fails, the cornea swells and becomes cloudy, as seen in bullous keratopathy. Such cases may need a bandage contact lens or penetrating keratoplasty (PK) — a full-thickness corneal graft.
If only partial layers are replaced, it’s called a lamellar keratoplasty.
Corneal Diseases: Keratoconus
Keratoconus is a chronic, progressive, non-inflammatory corneal ectasia (thinning disorder) that causes the normally round cornea to become cone-shaped. This irregular shape leads to irregular myopic astigmatism, blurred vision, and visual distortion.
Key features:
- Progressive thinning of the corneal stroma, especially at the apex.
- Cone formation due to localized ectasia.
- Seen in adolescence or early adulthood, often progressing slowly.
Diagnostic clues:
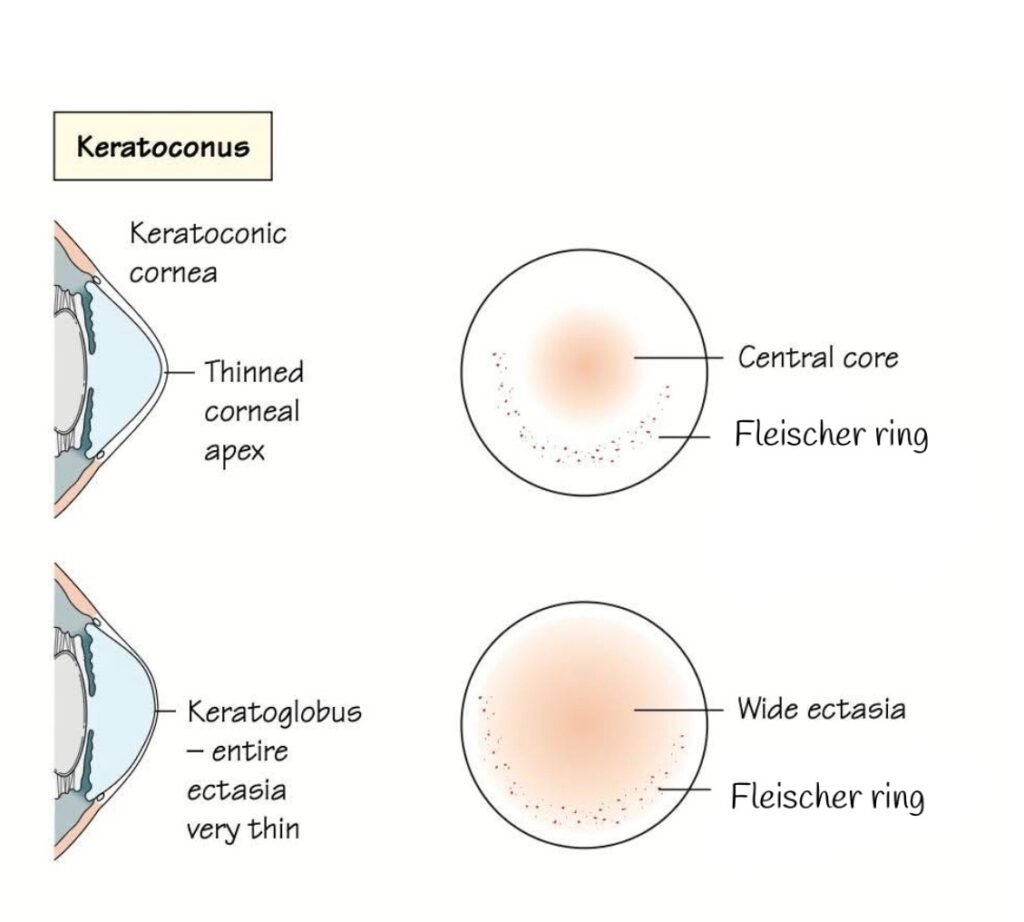
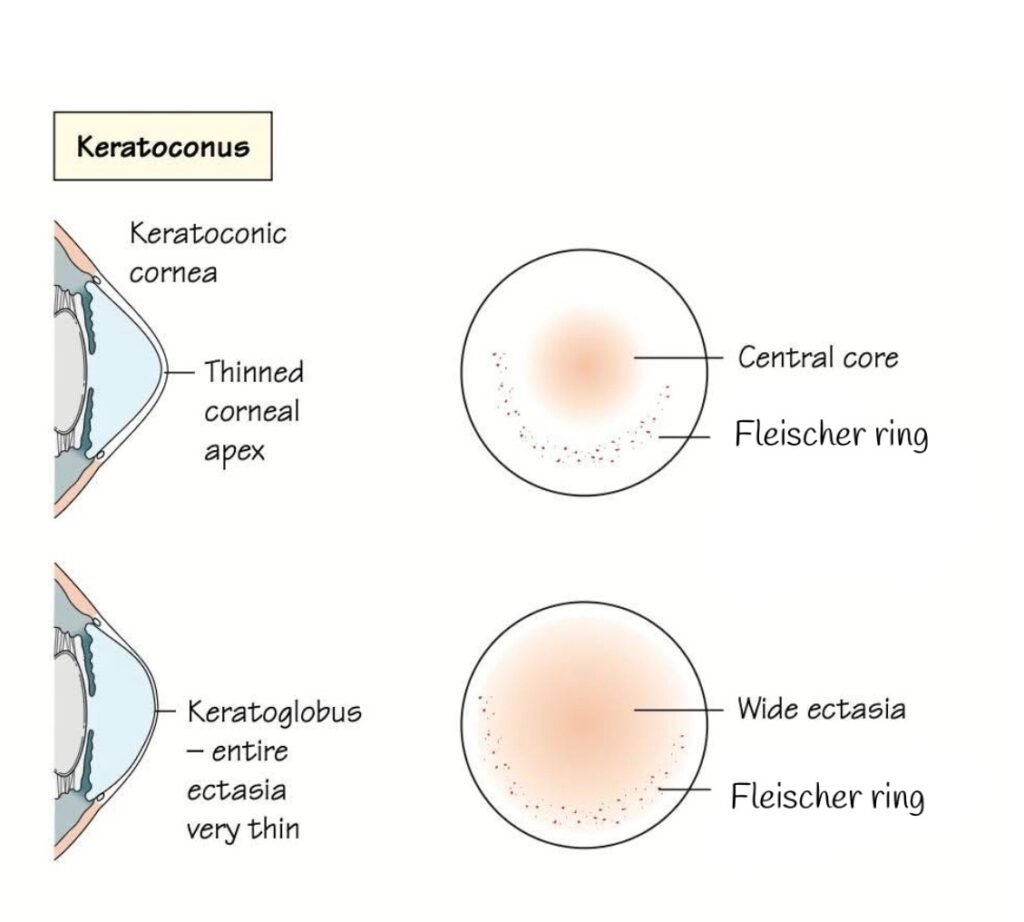
- Keratoconus:
- Shows a localized conical protrusion with a thinned corneal apex.
- The central core is steepened.
- A stromal Kaiser–Fleischer (K–F) ring may be seen on slit-lamp examination — this represents iron deposition in the corneal epithelium at the base of the cone.
- Keratoglobus:
- A more generalized corneal thinning and ectasia (entire cornea is thinned, not just the apex).
- The cornea appears globular rather than conical.
- The K–F ring can also be observed.
- This condition is rarer but more severe, with extreme corneal fragility.
Keratoconus vs Keratoglobus
| Feature | Keratoconus | Keratoglobus |
|---|---|---|
| Corneal shape | Cone-shaped, localized apex | Globular, generalized thinning |
| Area affected | Central or paracentral | Entire cornea |
| Onset | Adolescent or early adult | Congenital or early childhood |
| Thickness | Localized thinning | Uniform, very thin cornea |
| Complication risk | Moderate | High risk of perforation |
Management of Keratoconus
- Early stage: Spectacles or spherical/toric soft contact lenses (SPH CL).
- Moderate stage: Rigid gas permeable (RGP) lenses or scleral lenses for visual correction.
- Advanced stage: If scarring or extreme thinning develops, corneal cross-linking (CXL) to halt progression or penetrating keratoplasty (PK) for visual rehabilitation.
FAQ about Keratoconus
What is the Kaiser–Fleischer (K–F) ring?
The K–F ring is a circular brownish or golden ring seen at the edge of the cornea due to iron or copper deposition in the corneal layers. In keratoconus, the Fleischer ring (iron deposition at the cone’s base) is commonly observed under slit-lamp examination.
Is the Kaiser–Fleischer ring the same as the Fleischer ring?
No.
- The Fleischer ring appears in keratoconus due to iron deposits (hemosiderin) in the corneal epithelium.
- The Kaiser–Fleischer ring, on the other hand, is seen in Wilson’s disease, resulting from copper deposition at Descemet’s membrane.
How is keratoconus diagnosed?
Diagnosis is made using:
- Keratometry for measuring corneal curvature.
- Corneal topography for detecting early cone formation.
- Slit-lamp examination to visualize Fleischer ring or Vogt’s striae.
Is keratoconus hereditary?
Yes, there is often a genetic component, and it can run in families. Environmental factors like eye rubbing, allergies, and chronic irritation may accelerate progression.
