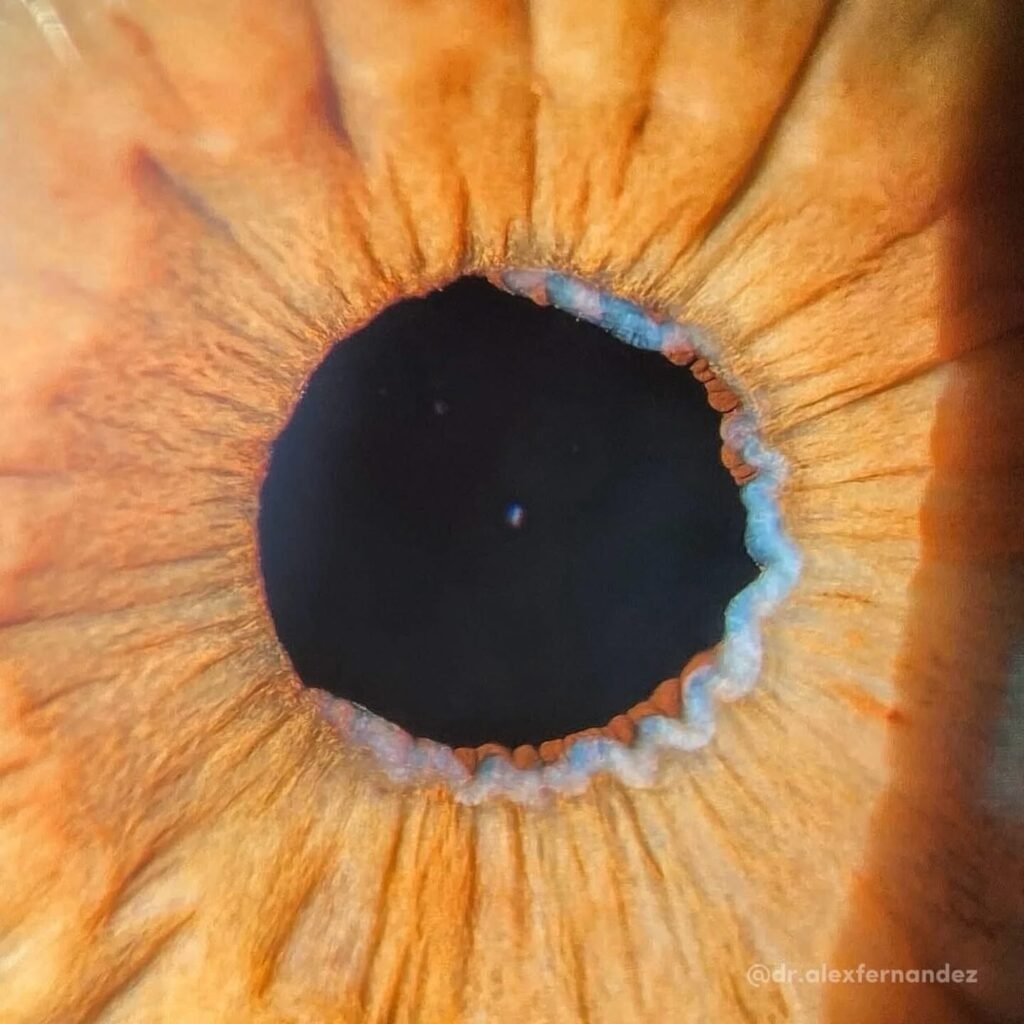
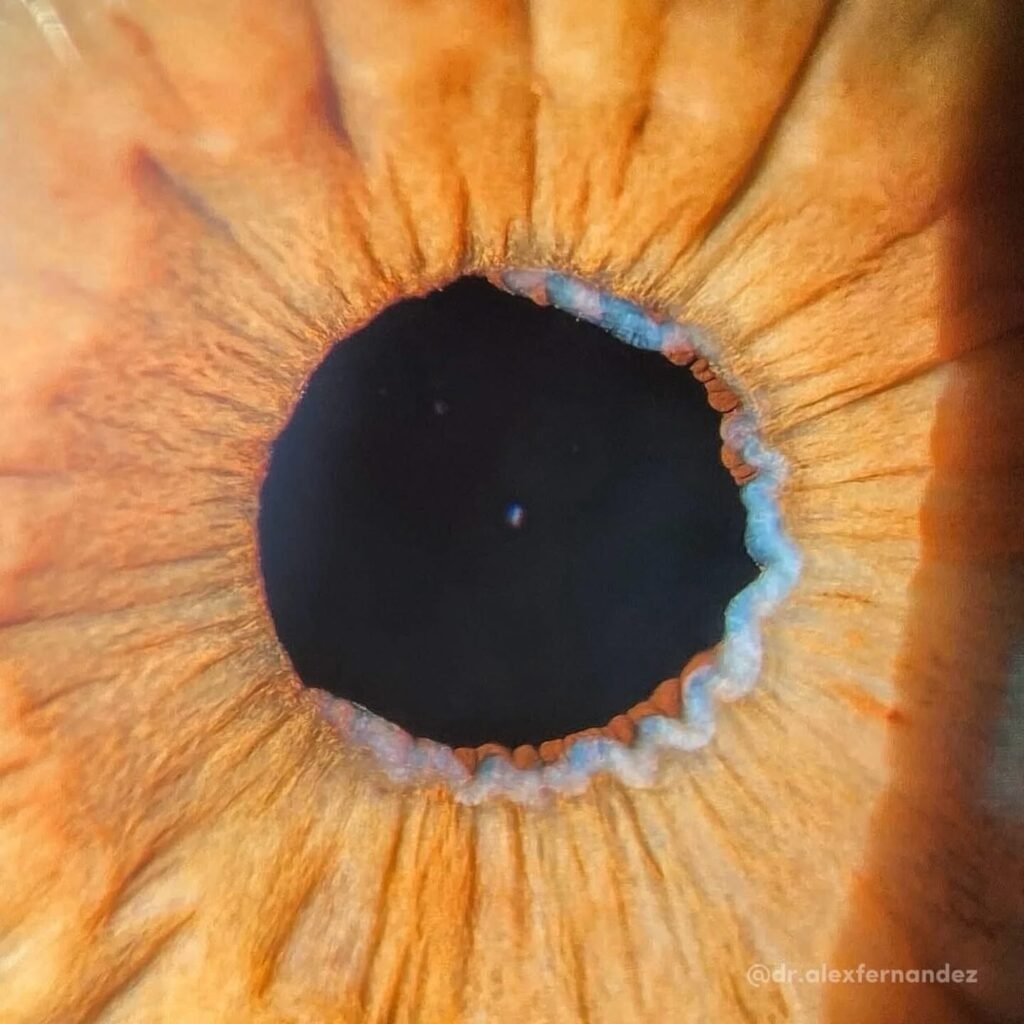
Pseudoexfoliation Syndrome (PEX): Recognizing the Pupillary Warning Signs
Pseudoexfoliation syndrome (PEX) is an age-related, systemic microfibrillopathy characterized by the progressive accumulation of abnormal white, dandruff-like fibrillar material within the anterior segment of the eye. Although classically identified on the anterior lens capsule, deposits are frequently visible at the pupillary margin, making careful slit-lamp evaluation essential.
This seemingly subtle material carries significant clinical implications — from impaired pupillary function to increased risk of glaucoma and intraoperative complications.
Pathophysiology and Anterior Segment Involvement
Pseudoexfoliation material is produced by abnormal extracellular matrix metabolism and accumulates in multiple ocular structures, including:
- Pupillary margin (iris ruff)
- Anterior lens capsule (often forming a central disc with a peripheral granular ring)
- Iris surface
- Zonular fibers
- Ciliary body
- Trabecular meshwork
The accumulation of this material leads to progressive structural and functional changes in the anterior segment.
Key Pupillary Findings in PEX
1. Characteristic Appearance
A hallmark sign is the deposition of white, flaky fibrillar material along the pupillary margin. This may also be seen as a concentric ring on the anterior lens capsule.
In some patients, the pupillary deposits may precede the classic lens findings and represent the earliest visible clue.
2. Iris Changes and Pigment Dispersion
PEX causes mechanical and structural disruption of the iris pigment epithelium, leading to:
- Liberation of iris pigment
- Pigment dispersion into the anterior chamber
- Increased trabecular meshwork pigmentation
- Iris transillumination defects
Transillumination defects occur due to damage to the iris pigment epithelium, allowing light to pass through areas of thinning.
3. Poor Pupillary Dilation
Patients with PEX frequently exhibit poor or rigid pupil dilation, often described clinically as a “non-dilating pupil.”
This occurs due to:
- Fibrotic changes in the iris sphincter
- Structural rigidity of the iris
- Progressive atrophy of the pupillary ruff
This feature becomes particularly significant during cataract surgery.
Clinical Significance
Increased Risk of Glaucoma
Pseudoexfoliation syndrome is the most common identifiable cause of secondary open-angle glaucoma worldwide.
Pseudoexfoliative glaucoma is typically:
- More aggressive
- Associated with higher intraocular pressure (IOP)
- Characterized by greater diurnal fluctuation
- Faster progressing than primary open-angle glaucoma
Importantly, glaucoma may develop even in patients who initially present with normal IOP.
Increased Cataract Surgery Risk
PEX significantly increases intraoperative risk due to:
- Zonular weakness
- Phacodonesis
- Capsular instability
- Poor dilation
- Higher risk of capsular rupture and vitreous loss
Preoperative identification allows surgeons to anticipate complications and adjust surgical technique accordingly.
Management and Follow-Up
Management of pseudoexfoliation syndrome centers on vigilant monitoring rather than immediate intervention in asymptomatic cases.
Recommended care includes:
- Annual comprehensive eye examinations
- Regular intraocular pressure measurement
- Optic nerve assessment
- Visual field testing when indicated
- Gonioscopy to assess angle pigmentation
Even in the absence of elevated IOP, the presence of pseudoexfoliation material warrants lifelong surveillance due to the increased risk of glaucoma development.
Clinical Takeaway
The presence of white fibrillar material at the pupillary margin signals a progressive condition with implications for glaucoma risk, iris integrity, and surgical safety.
Recognizing these pupillary signs early allows timely monitoring, appropriate counseling, and safer surgical planning.
Clinical Takeaway
Pseudoexfoliation syndrome is a progressive condition with structural and functional consequences. When deposits are visible at the pupillary margin, they should not be dismissed as incidental.
A thin, flaky line at the iris edge may represent a lifelong risk of glaucoma, increased surgical complexity, and the need for closer follow-up. Recognizing pupillary pseudoexfoliation is not about finding something unusual — it is about preventing something serious.
References
- Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45(4):265–315.
- Schlötzer-Schrehardt U, Naumann GOH. Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol.2006;141(5):921–937.
- Schlötzer-Schrehardt U. Pseudoexfoliation syndrome and glaucoma. Prog Retin Eye Res. 2018;67:1–29.
- Shingleton BJ et al. Outcome of phacoemulsification in eyes with pseudoexfoliation syndrome. J Cataract Refract Surg. 2003;29:1080–1086.
- Mitchell P et al. Pseudoexfoliation and the 5-year incidence of open-angle glaucoma. Ophthalmology.1999;106:2012–2016.
Follow us in facebook
