Iris Arteriovenous Malformation (AVM)
Iris vascular lesions can often raise concern for malignancy or serious ocular disease. Among these, iris arteriovenous malformation (AVM) is a rare but important benign condition that clinicians must recognize. Although it may appear alarming on slit-lamp examination, iris AVM is typically non-progressive and carries an excellent prognosis. Proper understanding helps prevent unnecessary interventions and ensures appropriate monitoring.
Management
Since iris AVMs are benign, non-progressive lesions, the treatment of choice is observation with periodic follow-up.
What Is Iris Arteriovenous Malformation?
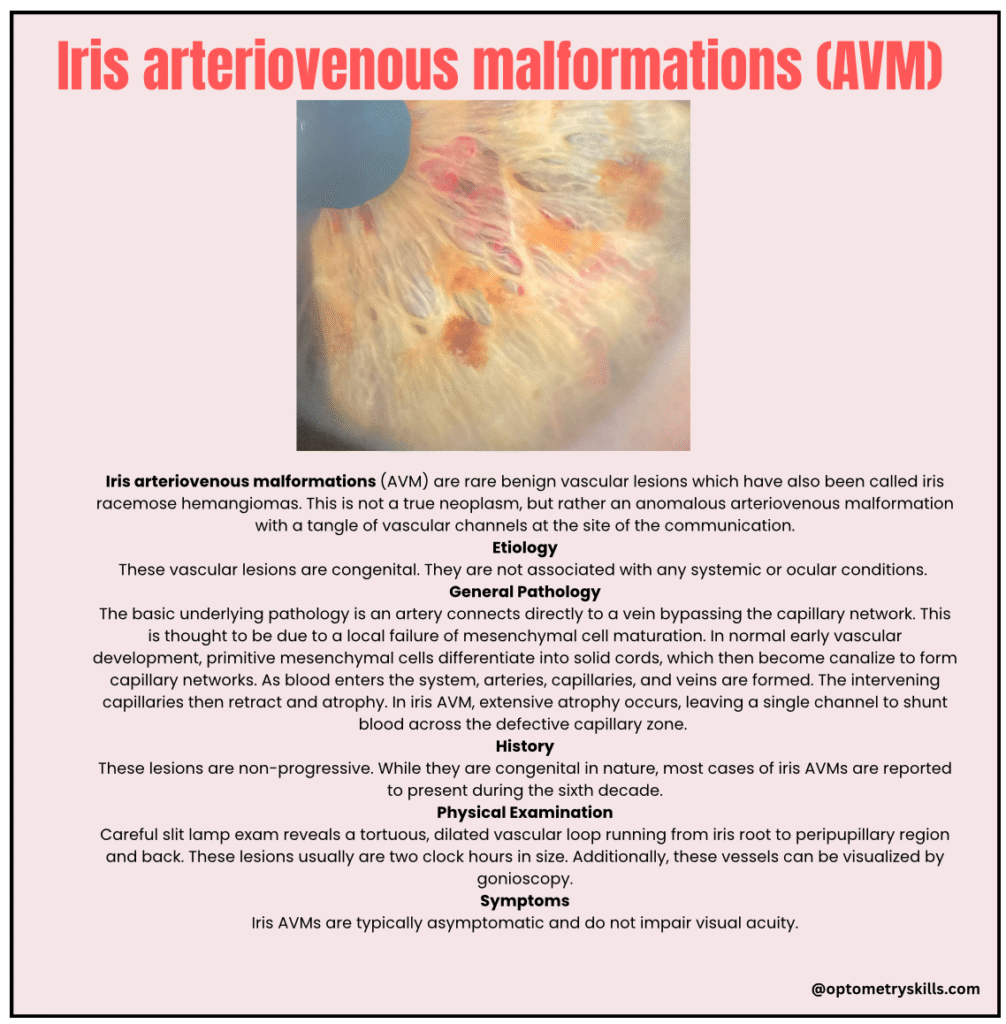
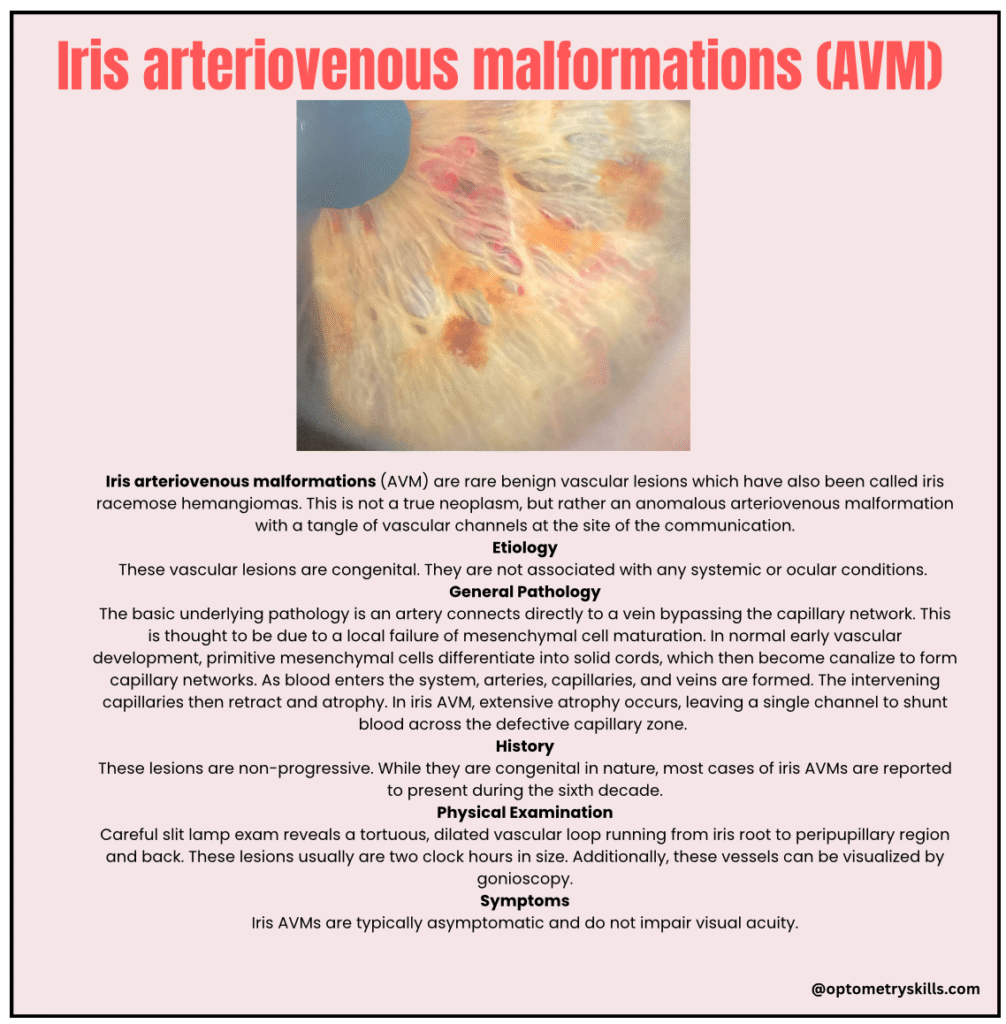
Iris arteriovenous malformation (AVM), also known as iris racemose hemangioma, is a rare benign vascular anomaly of the iris.
It is not a true neoplasm. Instead, it represents an abnormal direct communication between an artery and a vein, forming a tangled vascular channel without an intervening capillary bed.
Etiology
- Congenital in origin
- Not associated with systemic disease
- Not associated with other ocular conditions
- Non-progressive in nature
Although congenital, most reported cases present clinically in the sixth decade of life.
General Pathology
The underlying defect involves:
- Direct connection between an artery and a vein
- Absence of normal capillary network
Developmental Basis
During normal embryologic vascular development:
- Primitive mesenchymal cells form solid cords
- These canalize to create capillary networks
- Arteries, capillaries, and veins differentiate
- Redundant capillaries regress
In iris AVM:
- Excessive capillary atrophy occurs
- A single persistent vascular channel remains
- Blood shunts directly across the defective capillary zone
Pathophysiology
On microscopic examination, iris AVMs appear as:
- Telangiectatic vascular channels
- Lined by endothelial cells
- Lacking normal capillary intermediates
This explains the rapid blood flow and absence of leakage on angiography.
Clinical Features
History
- Congenital but often detected later in life
- Non-progressive
- Usually discovered incidentally
Symptoms
- Typically asymptomatic
- No effect on visual acuity
Physical Examination
On slit-lamp examination:
- Tortuous, dilated vascular loop
- Extends from iris root to peripupillary region and back
- Usually spans about two clock hours
- May be visualized on gonioscopy
A scleral sentinel vessel may sometimes be present, requiring exclusion of underlying malignancy.
Diagnostic Evaluation
Clinical Diagnosis
Diagnosis is usually made clinically through careful slit-lamp examination.
Fluorescein Angiography (FA)
Findings include:
- Rapid filling hyperfluorescence
- No late leakage
- Intervening iris hypoperfusion
Indocyanine Green Angiography (ICG)
- Useful in darkly pigmented irises
- Better penetration through pigmentation
- May show minimal leakage
Differential Diagnosis
Careful differentiation is essential.
Conditions to Consider
- Iris hemangioma
- Pathologic neovascularization of the iris
- Dilated normal vessels due to chronic inflammation
- Dilated vessels secondary to malignancy
- Iris varix
Ref : Retina images and Eyewiki,American Academy of Ophthalmology. Basic and Clinical Science Course, Section 2. Fundamentals and Principles of Ophthalmology. San Francisco: American Academy of Ophthalmology; 2023-2024., American Academy of Ophthalmology. Basic and Clinical Science Course, Section 4. Ophthalmic Pathology and Intraocular Tumors. San Francisco: American Academy of Ophthalmology; 2023-2024.
