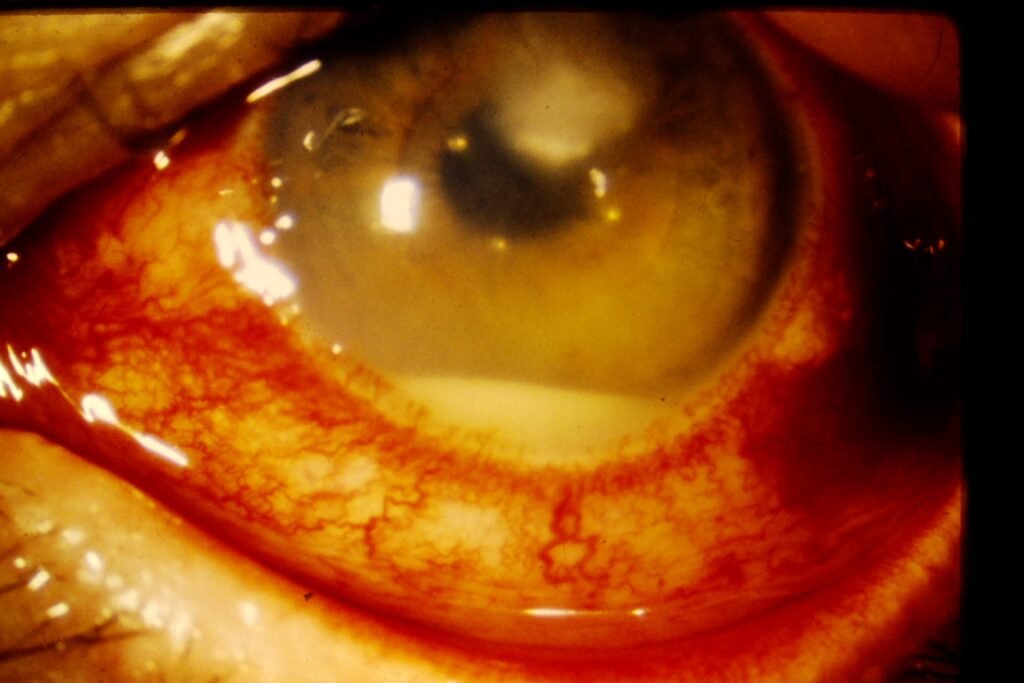
When a white fluid level appears inside the anterior chamber, it becomes an ophthalmic emergency.
This finding is called hypopyon, and when associated with a corneal infection, the condition is termed a hypopyon corneal ulcer.
It indicates a severe microbial keratitis where infection has penetrated deep into the cornea and inflammatory cells have collected inside the eye. Immediate recognition and treatment are critical to prevent permanent blindness.
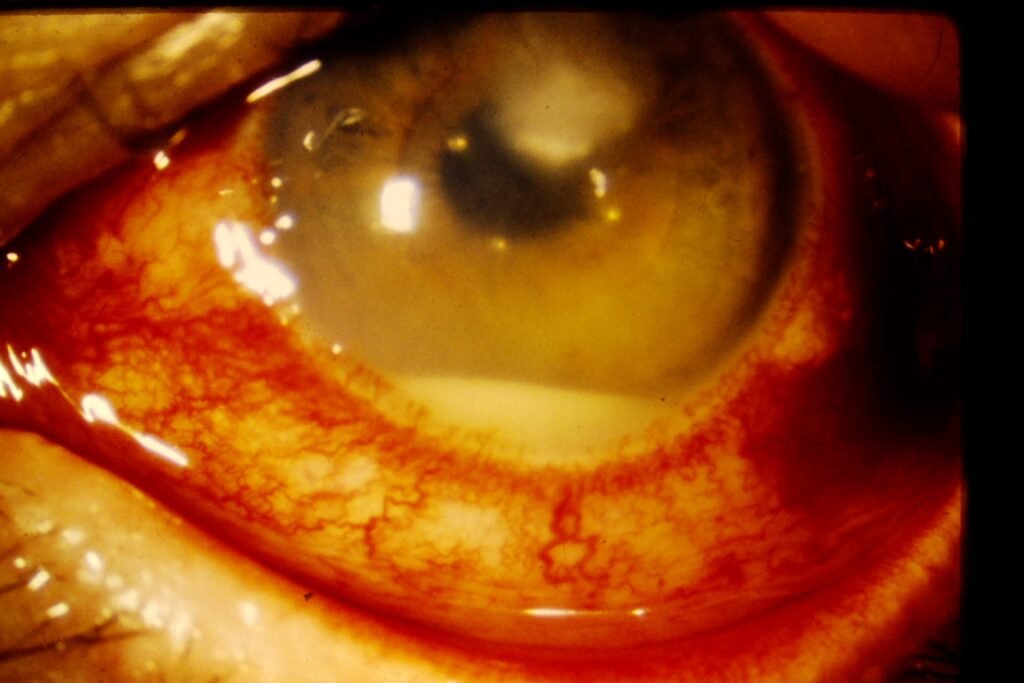
A hypopyon corneal ulcer is severe infectious keratitis accompanied by accumulation of leukocytes (pus) in the anterior chamber.
The hypopyon forms because inflammatory cells migrate from iris and ciliary body vessels due to intense corneal infection.
Why Does Hypopyon Form?
When bacteria or fungi invade the corneal stroma:
- Toxins and enzymes destroy corneal tissue
- Intense inflammation develops
- Leukocytes enter anterior chamber
- Gravity causes cells to settle inferiorly → visible white meniscus
This is a sterile inflammatory hypopyon, not always a direct intraocular infection (unlike endophthalmitis).
Causes of Hypopyon Corneal Ulcer
Bacterial (Most common emergency cause)
- Pseudomonas aeruginosa (contact lens wearers)
- Streptococcus pneumoniae
- Staphylococcus aureus
Fungal
- Aspergillus
- Fusarium
(Especially after trauma with vegetative matter)
Others
- Acanthamoeba (rarely forms hypopyon early)
- Severe marginal keratitis (rare)
Symptoms
- Severe eye pain
- Redness
- Watering and discharge
- Photophobia
- Sudden decrease in vision
- Difficulty opening eye
Clinical Signs
Corneal Findings
- Large stromal infiltrate
- Epithelial defect (stains with fluorescein)
- Surrounding edema
- Possible corneal thinning
Anterior Chamber Findings
- Visible layered hypopyon
- Cells and flare
- Ciliary congestion
Differentiating Bacterial vs Fungal Hypopyon Ulcer
| Feature | Bacterial Ulcer | Fungal Ulcer |
|---|---|---|
| Onset | Rapid | Gradual |
| Pain | Severe | Moderate |
| Margins | Well defined | Feathery margins |
| Surface | Suppurative | Dry, rough |
| Hypopyon | Mobile | Fixed, immobile |
| Satellite lesions | Absent | Present |
| History | Contact lens | Trauma with plant matter |
Diagnosis
- Slit lamp examination
- Fluorescein staining
- Corneal scraping for Gram stain and KOH mount
- Culture and sensitivity
References
American Academy of Ophthalmology (AAO) – Bacterial Keratitis Preferred Practice Pattern
https://www.aao.org
Kanski & Bowling. Clinical Ophthalmology: A Systematic Approach, 9th Edition
WHO Guidelines for Management of Microbial Keratitis
https://www.who.int
