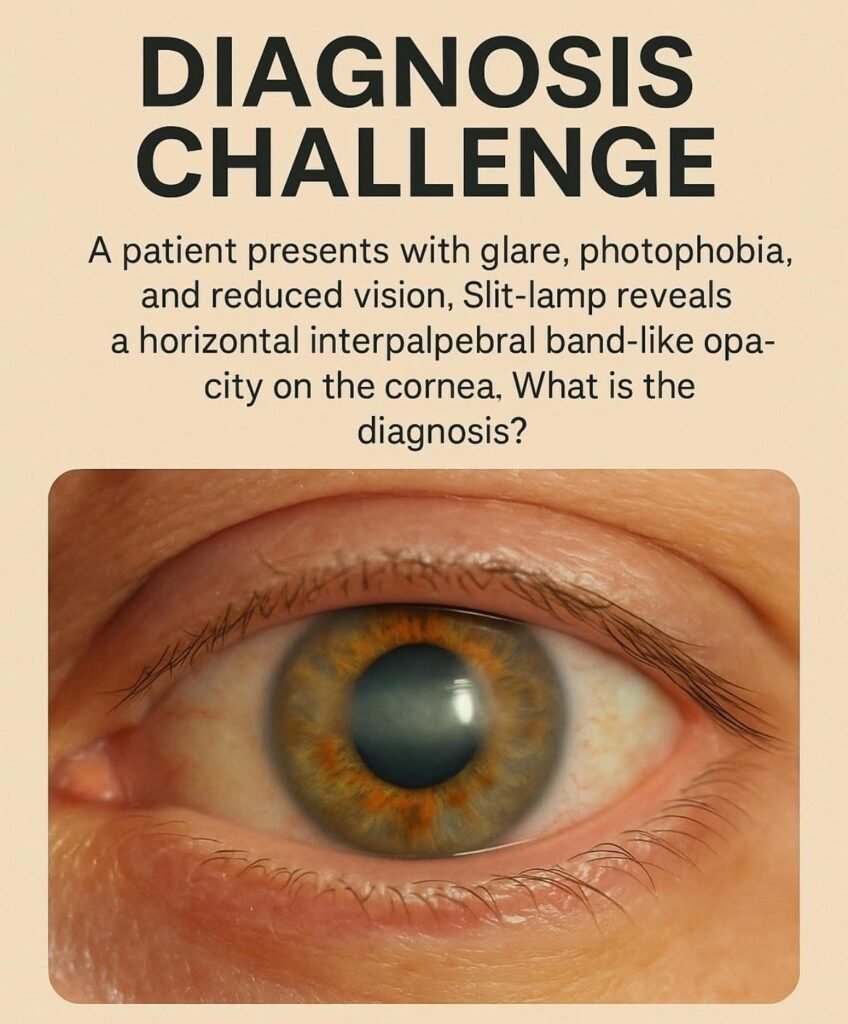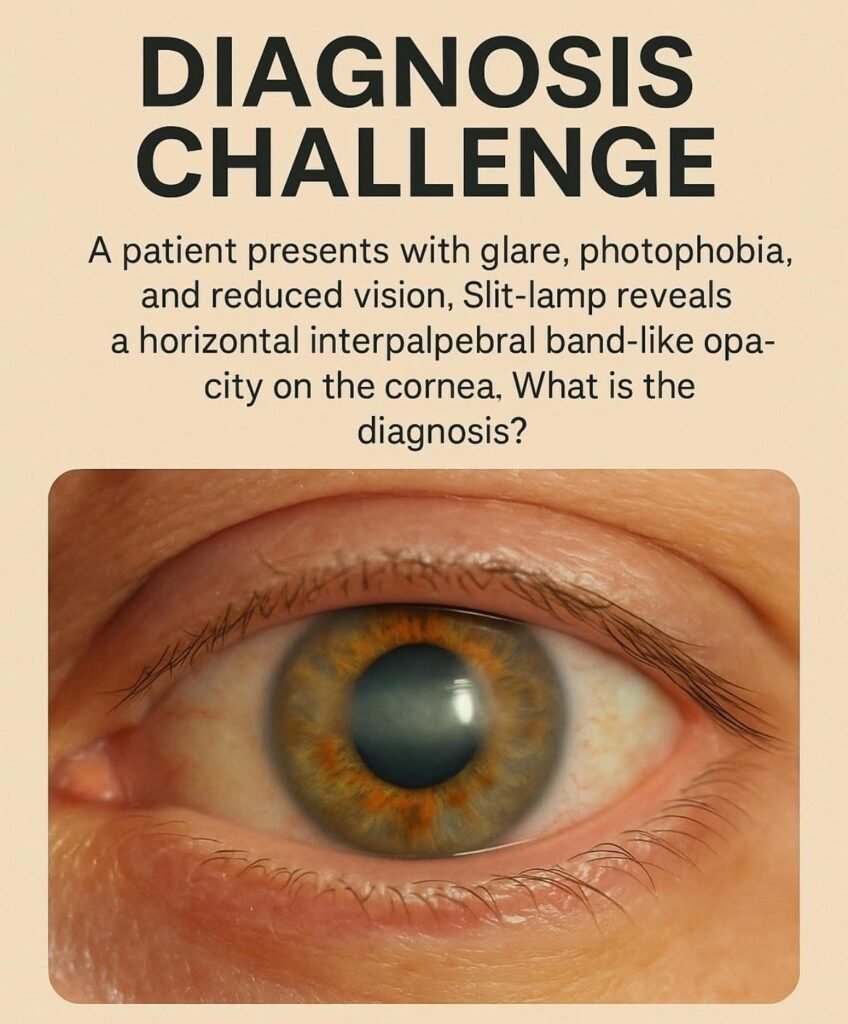
Calcific Band Keratopathy: Key Clinical Insights for Optometrists
What is Calcific Band Keratopathy?
Calcific Band Keratopathy (CBK) is a degenerative corneal condition characterised by calcium hydroxyapatite deposition in the:
- Bowman’s layer
- Epithelial basement membrane
- Superficial anterior stroma
The deposits form a horizontal, interpalpebral, band-like opacity across the cornea — hence the name band keratopathy.
Why It Matters for Optometrists
Optometrists are often the first point of contact for these patients. Recognising CBK enables timely referral, improves comfort, and prevents visual decline.
Clinical Presentation
Symptoms
- Decreased visual acuity (gradual)
- Glare & photophobia
- Foreign-body sensation
- Tearing or irritation
Signs on Slit-Lamp
- Horizontal band opacity across interpalpebral zone
- Begins at 3 and 9 o’clock and spreads centrally
- Surface may appear rough and plaque-like
- Lucid interval at limbus
- Advanced cases: epithelial breakdown, pain
Pearl: CBK typically spares the superior and inferior cornea, as they are protected by the eyelids.
Differential Diagnosis
| Condition | Key Difference |
|---|---|
| Salzmann’s Nodular Degeneration | Elevated bluish-white nodules |
| Lipid Keratopathy | Associated vascularisation, lipid deposits |
| Spheroidal Degeneration | Golden, oily granules; pinguecula-like |
| Band-shaped Keratopathy post trauma | Localised to area of previous injury |
Etiology & Associations
CBK may be idiopathic but commonly associated with:
Ocular Causes
- Chronic uveitis (e.g., juvenile idiopathic arthritis)
- Chronic corneal edema
- Long-standing glaucoma
- Keratoconjunctivitis sicca
- Silicone oil after retinal surgery
- Phthisical eye
Systemic Causes
- Hypercalcemia (e.g., hyperparathyroidism)
- Chronic kidney disease
- Sarcoidosis
- Vitamin D toxicity
Clinical Reminder: Always evaluate systemic history when CBK is detected.
Investigations
For new or bilateral unexplained cases:
- Serum calcium & phosphate
- Parathyroid hormone levels
- Renal function tests
Ocular assessment:
- Slit-lamp magnification & optic section
- Fluorescein staining: highlights irregular surface
Management
Non-Surgical / Supportive
- Lubricating drops/ointments
- Bandage contact lenses for pain
- Avoid calcium-containing topical meds if possible
Definitive Treatment
| Treatment | Notes |
|---|---|
| EDTA chelation (gold standard) | Removes calcium; often excellent visual recovery |
| Superficial keratectomy | For deeper or dense plaques |
| PTK (Phototherapeutic Keratectomy) | If recurrence or deeper stromal involvement |
Referral: Refer to a corneal specialist for EDTA chelation/surgical removal.
Prognosis
- Vision often improves significantly post-treatment
- Recurrence possible, especially if underlying cause persists
Follow-Up Advice:
- Monitor ocular inflammation
- Support lubrication
- Address systemic conditions
Quick Summary for Students
| Feature | Description |
|---|---|
| Location | Interpalpebral zone, Bowman’s layer |
| Appearance | White-grey, band-like plaque |
| Symptoms | Glare, photophobia, decreased vision |
| Key Associations | Chronic uveitis, renal disease, hypercalcemia |
| Treatment | EDTA chelation +/- PTK |
Optometrist’s Take-Home Message
CBK is easy to overlook in early stages. Every slit-lamp exam is an opportunity to protect vision. Remember:
- Look for band-like calcium at 3 & 9 o’clock
- Ask about systemic & inflammatory conditions
- Provide early referral for chelation therapy
- Support the ocular surface to improve comfort
With proper recognition and timely intervention, patients can enjoy significant improvement in clarity and comfort.