What is CAIRS keratoplasty?
CAIRS stands for Corneal Allogenic Intrastromal Ring Segments. It’s a type of corneal transplant where human donor corneal tissue is placed inside the cornea in a ring-like fashion to strengthen and reshape it. This is a newer form of keratoplasty that uses allogenic (donor) tissue instead of synthetic rings.
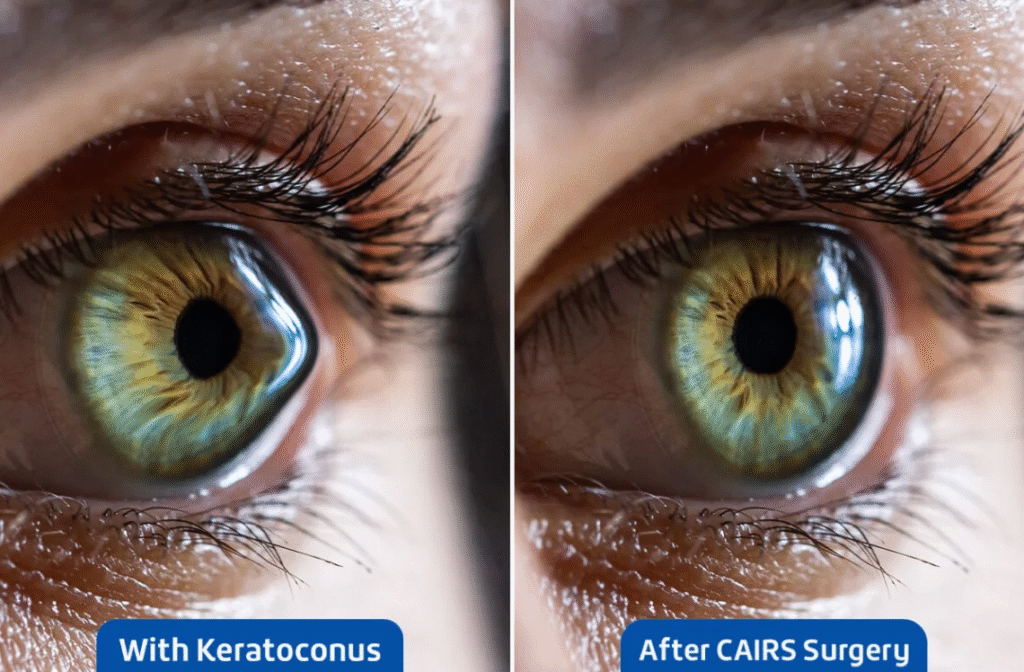
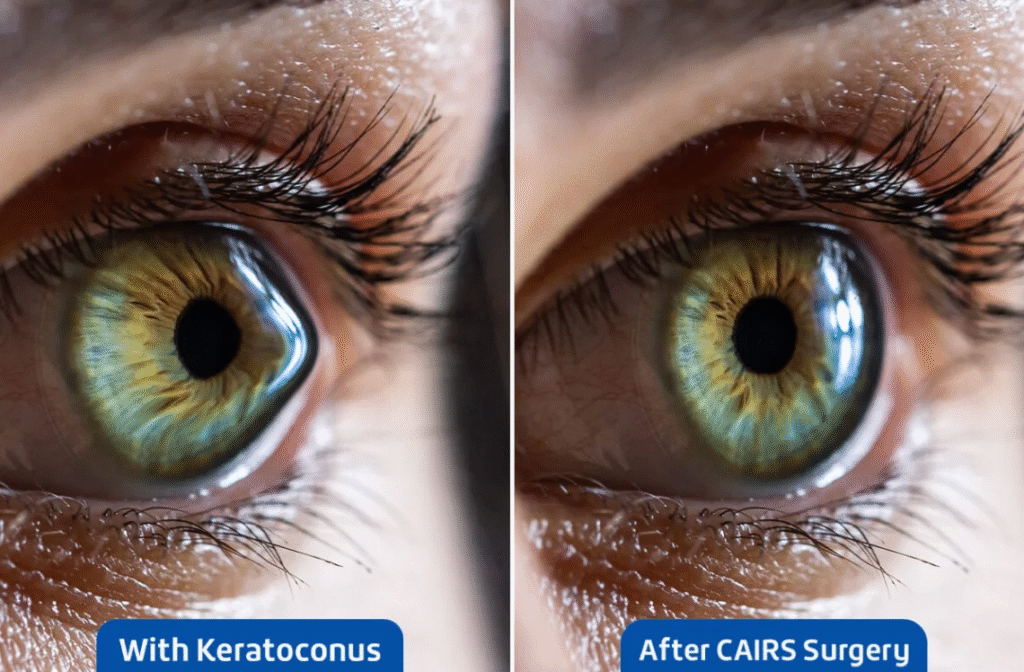
Corneal Allogenic Intrastromal Ring Segment Keratoplasty (CAIRS Keratoplasty) is a modern surgical technique used in the treatment of keratoconus. It involves implanting finely shaped pieces of donor corneal tissue into the corneal stroma to reinforce and reshape the weakened, ectatic cornea, thereby improving both corneal structure and visual clarity. Because CAIRS uses biological graft material and has demonstrated strong outcomes with a favourable safety profile, it is formally recognised as a corneal transplantation procedure by health funding authorities in Australia, the United Kingdom, Japan, Germany, Brazil, the Netherlands, and a number of other countries.
In contrast to traditional synthetic intrastromal corneal ring segments (ICRS) made from materials such as PMMA, CAIRS keratoplasty uses preserved allogeneic corneal tissue. This biological compatibility reduces the likelihood of complications sometimes seen with non-organic implants, including extrusion, infection, or chronic foreign body reaction.
The CAIRS technique was pioneered by Dr Soosan Jacob, who first introduced it in 2018 through a large case series published in the Journal of Refractive Surgery.
What are the main types of keratoplasty?
There are several approaches depending on which layer of the cornea needs treatment:
- Penetrating keratoplasty: Whole corneal thickness is replaced.
- Lamellar keratoplasty: Only part of the cornea is replaced (partial thickness), preserving healthy tissue.
Examples include: - CAIRS: donor tissue rings within the cornea to correct shape and strength while preserving surrounding tissue
How successful is CAIRS and corneal transplant surgery?
Traditional corneal transplants have a high success rate, with many patients achieving improved vision for many years. Newer techniques like CAIRS aim to reduce complications further, particularly in cases like keratoconus.
What are the risks and complications?
As with all surgeries, risks exist. They may include:
- graft rejection (when the immune system attacks the donor tissue),
- infection,
- inflammation,
- increased eye pressure (glaucoma),
- vision changes or astigmatism,
- detachment of graft tissue.
How long is recovery?
Recovery varies by procedure type:
- Partial-thickness techniques (like lamellar keratoplasty or CAIRS) often heal faster with fewer complications. Mayo Clinic
- Full-thickness transplants may take many months to a year for vision to stabilize and stitches to be removed. MedlinePlus
Your doctor will give specific guidance based on your eye condition.
Can the transplant fail?
Yes, graft failure can occur if problems like rejection or infection develop. If a graft fails, it may be possible to repeat the transplant or consider alternative treatments.
