Understanding Binocular Diplopia Examinations
Binocular diplopia, commonly known as double vision, occurs when both eyes fail to work together to create a single, unified image. It is an important clinical symptom that often signals a dysfunction in the ocular muscles, nerves, or binocular vision mechanisms. A structured examination helps eye care professionals pinpoint the underlying cause — whether it’s muscular, neurological, or psychogenic in nature.
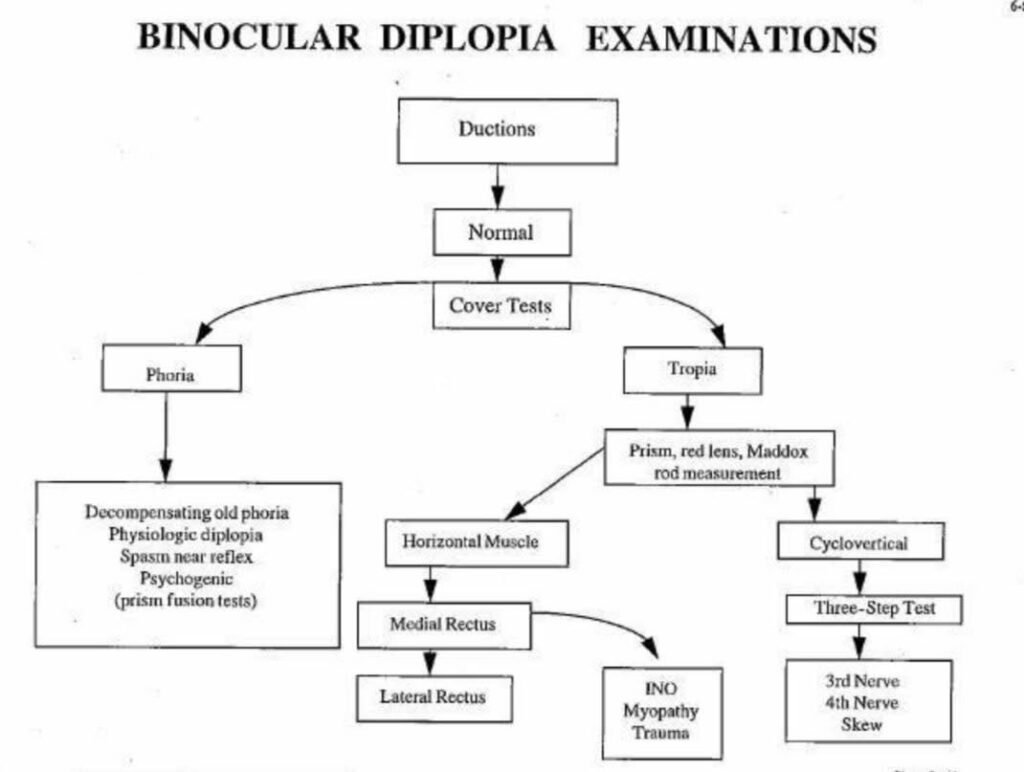
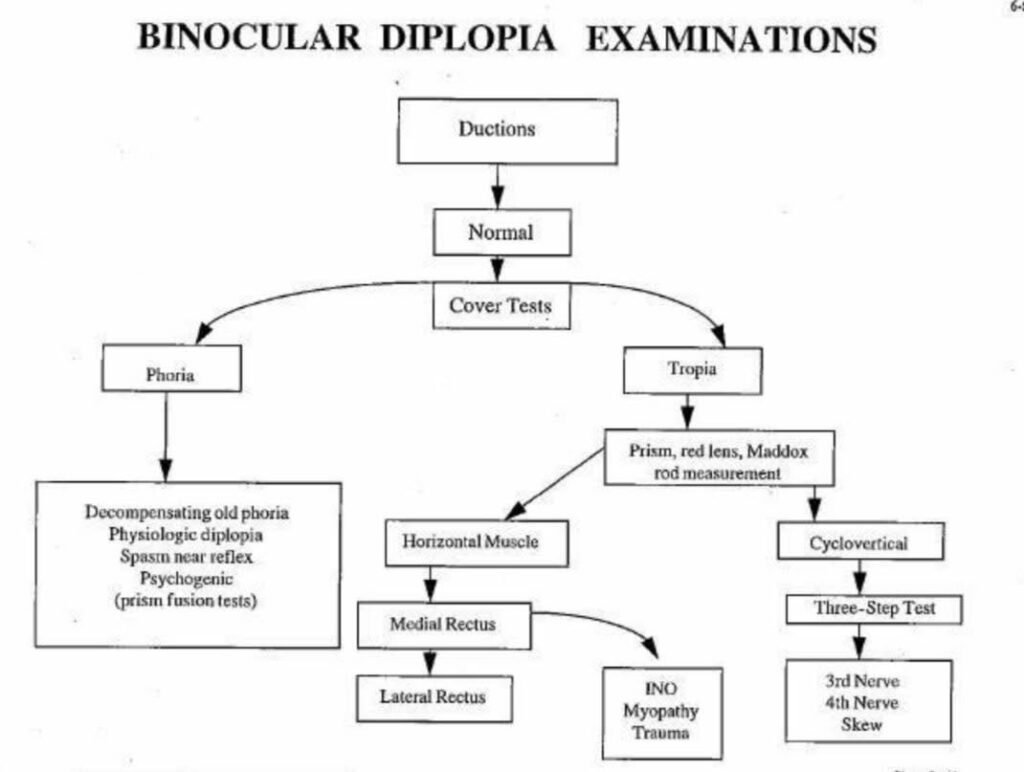
This article outlines the step-by-step approach to evaluating binocular diplopia, as represented in the diagnostic flowchart.
Step 1: Assessing Ocular Motility (Duction Tests)
The first step in examining a patient with binocular diplopia is to assess ductions — the movement of each eye individually. This helps determine if the extraocular muscles are functioning normally.
If ductions are normal: The problem likely lies in binocular coordination (not muscle paralysis). If ductions are limited: It may suggest a restrictive or paralytic muscle disorder, requiring further specific testing.
Step 2: Performing Cover Tests
When ductions are normal, the next step is cover testing to evaluate eye alignment and uncover hidden or manifest deviations.
Phoria: A latent deviation controlled by fusion. It becomes evident only when binocular vision is interrupted. Tropia: A manifest deviation present even when both eyes are open.
Step 3: Phoria Assessment
If a phoria is detected, the examiner must determine whether it is:
Decompensating old phoria: A previously controlled phoria that has broken down. Physiologic diplopia: A normal perceptual phenomenon. Spasm of near reflex: Excessive convergence or accommodation. Psychogenic diplopia: Vision disturbance due to psychological causes.
To confirm, prism fusion tests are used to assess the patient’s ability to maintain binocular single vision.
Step 4: Tropia Analysis
If the cover test indicates tropia, further differentiation is needed using specialized tools such as:
Prism bar testing Red lens test Maddox rod test
These tests help quantify and characterize the deviation, whether it’s horizontal or cyclovertical.
Horizontal Muscle Involvement
Horizontal deviations involve:
Medial Rectus (MR): Responsible for adduction.
Lateral Rectus (LR): Responsible for abduction.
Possible causes include:
Internuclear Ophthalmoplegia (INO): Due to a lesion in the medial longitudinal fasciculus. Myopathy: Muscle weakness from systemic or local diseases. Trauma: Mechanical injury to extraocular muscles.
Cyclovertical Muscle Involvement
Vertical or torsional diplopia is often more complex and involves cyclovertical muscles. The three-step test helps identify the affected muscle and associated cranial nerve.
The Three-Step Test
Determine which eye is hypertropic (higher). Assess whether the deviation increases with right or left gaze. Evaluate the deviation in head tilt to either shoulder.
This systematic test helps isolate the defective muscle and, consequently, the responsible cranial nerve:
- 3rd Nerve (Oculomotor) Palsy
- 4th Nerve (Trochlear) Palsy
- Skew Deviation (Brainstem cause)
Conclusion
Evaluating binocular diplopia requires a logical, stepwise approach — beginning from simple motility testing to advanced prism and neuro-ophthalmic evaluations. Correctly distinguishing between phoria and tropia, and further identifying the involved muscle or nerve, is crucial for accurate diagnosis and management.
This systematic examination not only aids in differentiating benign causes like decompensating phorias from serious neurological pathologies but also ensures that patients receive timely and targeted treatment.
