Piggyback Contact Lenses (PBCL): what they are, when we use them
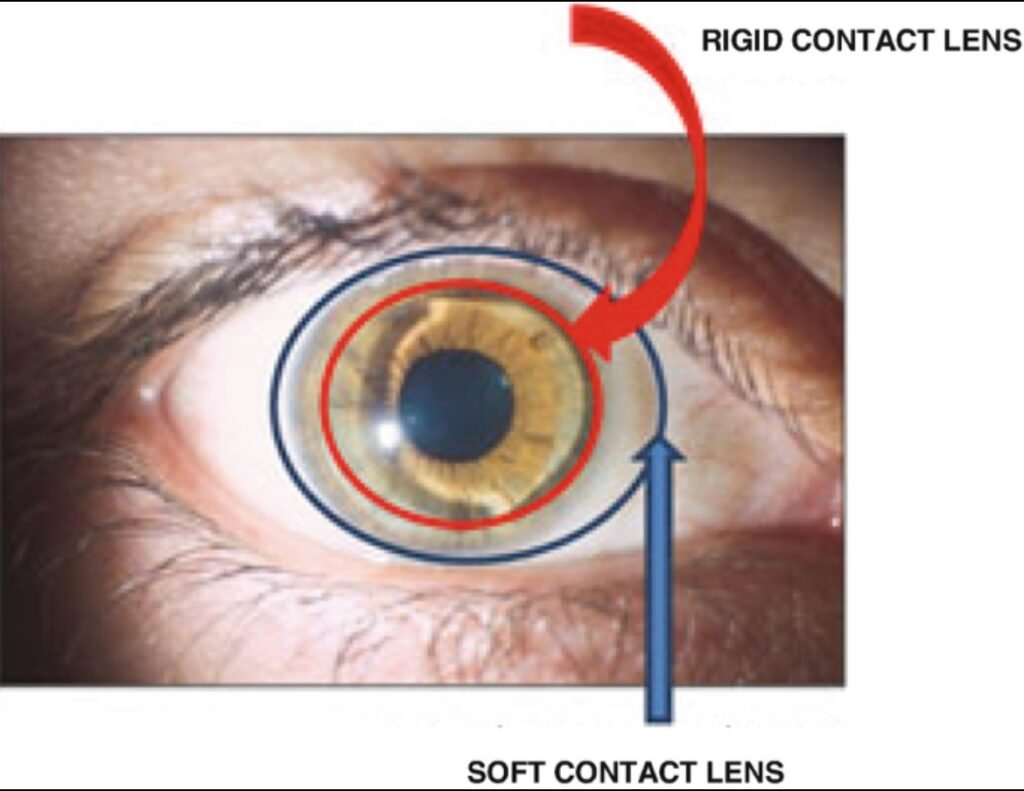
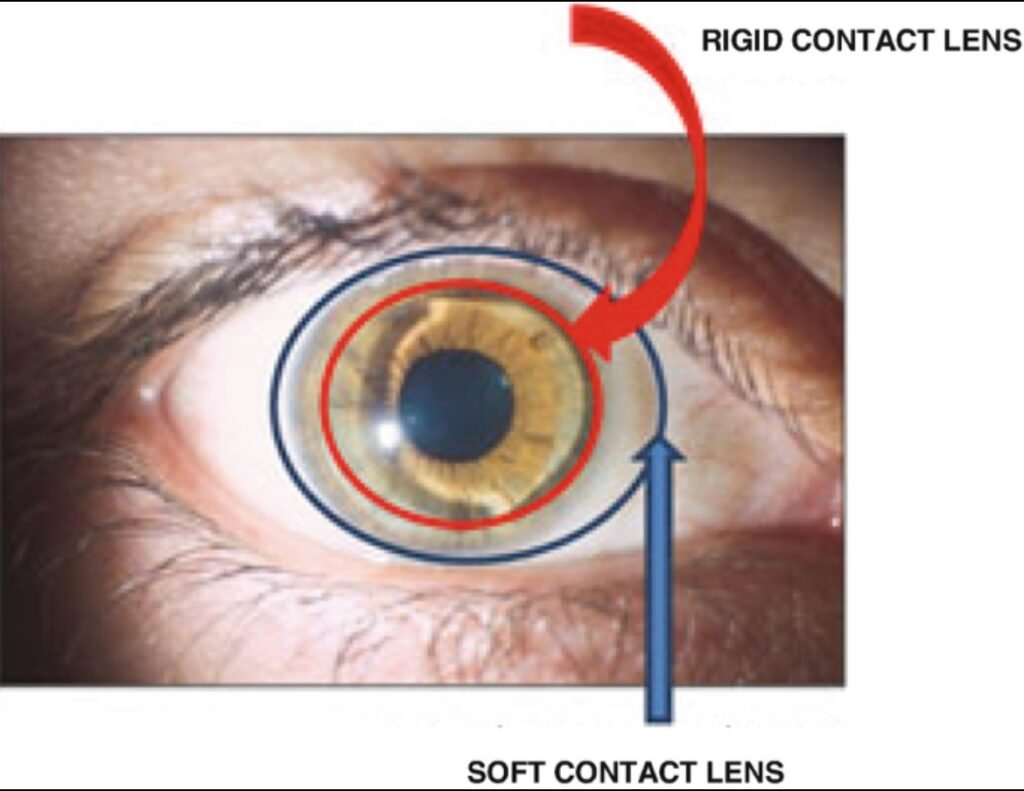
Piggyback contact lens systems (often abbreviated PBCL) pair two lenses on the same eye: a soft contact lens as a “carrier” or cushion, and a rigid gas-permeable (RGP) lens placed on top. This approach aims to keep the excellent optics of RGP lenses for highly irregular corneas while improving comfort and protecting the corneal surface. The technique has been used for decades and continues to be a practical tool when other lens types are unsuitable or have failed.
What exactly is a piggyback system?
A piggyback system typically consists of:
a high-oxygen soft contact lens (often silicone-hydrogel) placed directly on the cornea, and an RGP lens placed on top of that soft lens.
The soft lens smooths the anterior surface and cushions the RGP, improving tolerance, reducing mechanical irritation, and protecting fragile corneal epithelium. Modern high-Dk soft materials and oxygen-permeable GP materials have made PBCL safer than earlier combinations.
Main indications
PBCL are most commonly considered for:
Keratoconus and other corneal ectasias when RGPs provide the best optics but are intolerable because of discomfort. Recurrent corneal erosions or areas prone to epithelial breakdown where a cushion is protective. Patients with GP lens awareness or poor fit due to a steep/irregular apex (e.g., decentered cones) who nevertheless obtain good vision with GP optics.
PBCL can also be a useful intermediate strategy to delay or avoid corneal surgery in selected patients.
How practitioners fit piggyback systems (practical points)
Start with the soft lens choice. Many fitters use a high-oxygen disposable silicone-hydrogel lens (plano or low power), which acts as a cushion and maintains oxygen transmission. Some practitioners choose a low negative power soft lens to slightly flatten the anterior optical surface—this can influence GP power. Select the RGP next. Fit the RGP as you would normally, but over the soft lens: centration, movement and fluorescein pattern must be assessed through the soft lens. Some adjust RGP base curve or power because the soft lens changes the anterior radius. Evaluate oxygen delivery. Using high-Dk materials for both lenses and limiting wearing time initially reduces hypoxia risk. Regular follow-up and monitoring for corneal edema or neovascularization are essential.
Benefits — why choose PBCL?
Best of both worlds: RGP optics (sharp vision on irregular cornea) with the comfort and protection of a soft lens. Improved tolerance and wear time for patients otherwise unable to tolerate RGPs. Clinical reports show improved comfort and, in many cases, equal or better visual acuity compared with RGP alone. Alternative to surgery in some patients who want to postpone corneal procedures.
Risks and common complications
Giant papillary conjunctivitis (GPC) — allergic papillary response to the increased lens surface and deposits is a known cause of PBCL failure in some reports.
Lens handling complexity and hygiene burden — two lenses require more handling, which can increase the chance of contamination or disinfection errors.
Hypoxia/corneal edema — although reduced with modern high-Dk materials, oxygen transmission remains an important consideration; careful material selection and follow-up are mandatory.
Cost and maintenance — higher ongoing cost and clinic time (fitting fees, adjustments, replacements) compared with single-lens solutions.
Alternatives to piggyback systems
When PBCL are unsuitable or fail, common alternatives include:
Scleral lenses — vault the cornea and rest on the sclera, providing excellent optics and comfort for many irregular corneas; increasingly favored because of comfort and reduced mechanical contact with the cornea. Scleral lenses have strong evidence for safety and efficacy in keratoconus. Hybrid lenses — rigid center with a soft skirt, designed to combine GP optics and soft comfort in a single lens; may be helpful but have their own fitting and durability considerations. Customized RGPs or aspheric designs — in some cases, modification of the GP design alone can improve comfort and optics without doubling lenses.
Practical advice for patients (what to expect)
Expect an adjustment period to learn insertion/removal for two lenses; start with shorter wear times and increase gradually as advised. Keep strict hygiene: follow the practitioner’s cleaning/disinfection for both lenses. Use only prescribed solutions — rinsing with tap water or homemade solutions is unsafe. Attend regular follow-up visits to monitor corneal health (look for redness, pain, blurred vision, or sudden changes). Promptly report discomfort, sudden vision change, or discharge.
Summary
Piggyback contact lens systems remain a valuable, evidence-based option when RGP optics are needed but comfort or corneal protection is problematic. With modern high-Dk materials and careful fitting, PBCL can restore useful vision and prolong comfortable lens wear for patients with keratoconus, recurrent erosions, or other irregular corneas. However, alternatives such as scleral or hybrid lenses may be preferable in many cases; the choice should be individualized after discussing risks, benefits, and lifestyle considerations with a skilled contact lens practitioner.
Selected references and further reading (sources used)
Rathi VM, et al. Contact lens in keratoconus. Indian J Ophthalmol. 2013. (review discussing PBCL and other options). Şengör T. Update on Contact Lens Treatment of Keratoconus. Review (2020). (modern perspective including scleral preference). Sengor T, et al. High Dk piggyback contact lens system for … (PMC article describing modern PBCL materials and oxygen considerations). Fuller DG, et al. Safety and Efficacy of Scleral Lenses for Keratoconus. (PMC 2020) — for comparison of alternatives. American Academy of Ophthalmology — Corneal Ectasia Preferred Practice Pattern (guidance document; includes PBCL mention and monitoring needs).
