Key Ocular Parameters Relevant to Primary Angle-Closure Glaucoma (PACG)
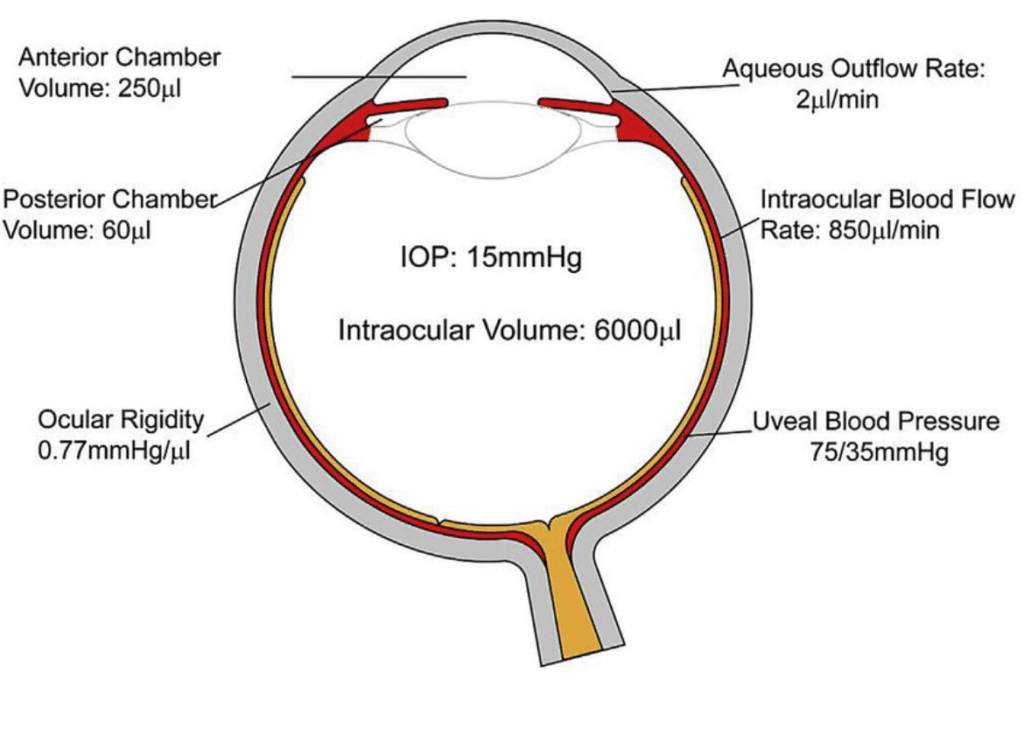
Understanding the anatomical and physiological characteristics of the eye is crucial in identifying patients at risk of Primary Angle-Closure Glaucoma (PACG). The schematic illustration highlights several critical intraocular parameters — including ocular volume, aqueous dynamics, blood flow, and ocular rigidity — that influence intraocular pressure (IOP) and angle anatomy.
PACG develops when the anterior chamber angle narrows, obstructing aqueous humor drainage and causing IOP elevation. Recognizing the anatomical predispositions that contribute to this process supports early detection and intervention.
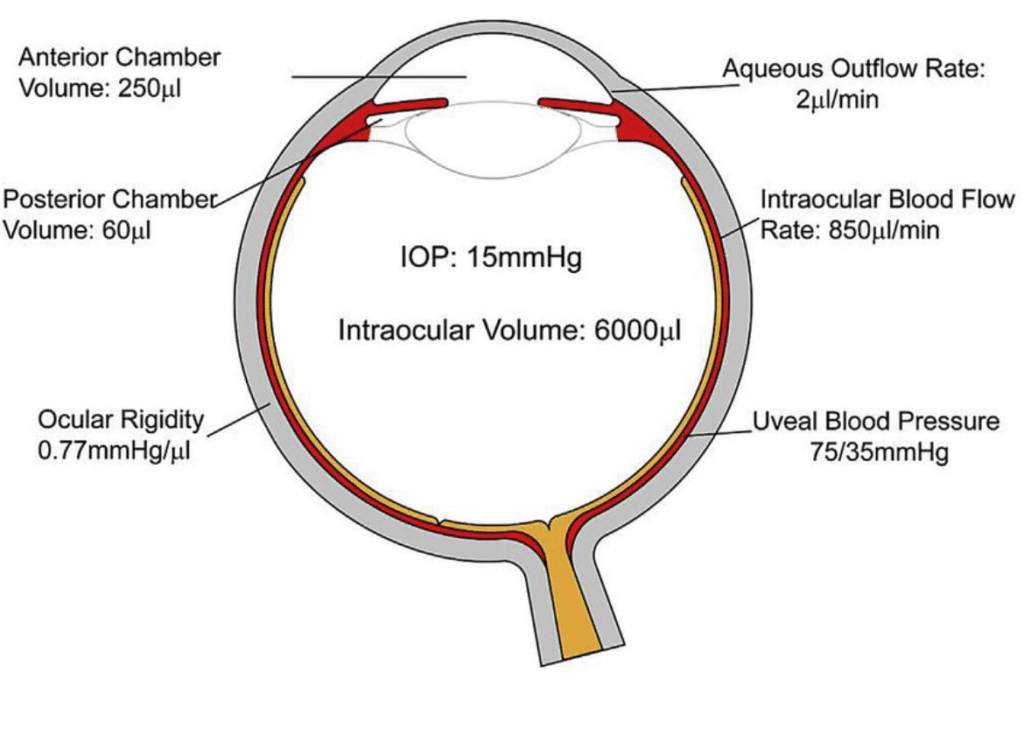
1. Intraocular Pressure (IOP)
- Normal IOP: ~15 mmHg
- Maintained through a balance between aqueous humor production and outflow
In PACG, pupillary block or angle crowding impairs outflow, causing pressure buildup.
2. Intraocular Volume
- Total intraocular volume: ~6000 μl
- Anterior chamber volume: ~250 μl
- Posterior chamber volume: ~60 μl
A smaller anterior chamber volume is a hallmark PACG risk factor, commonly seen in hyperopic eyes and aging lenses.
3. Aqueous Humor Flow and Outflow
- Aqueous outflow rate: ~2 μl/min
Aqueous humor circulates from the posterior chamber → pupil → anterior chamber → trabecular meshwork → Schlemm’s canal.
Angle narrowing → outflow resistance → IOP rise
This mechanism is central in primary angle closure.
4. Intraocular Blood Flow
- Ocular blood flow rate: ~850 μl/min
- Uveal blood pressure: ~75/35 mmHg
Uveal circulation contributes to ocular nourishment and pressure dynamics. In PACG, perfusion may be compromised during acute IOP spikes, threatening optic nerve health.
5. Ocular Rigidity
- Ocular rigidity coefficient: ~0.77 mmHg/μl
Ocular rigidity reflects the eye’s biomechanical response to volume change. Elevated rigidity can influence IOP spikes, whereas lower rigidity may mask early changes.
Why These Parameters Matter in PACG
| Parameter | PACG Relevance |
|---|---|
| Small anterior chamber | Angle crowding, pupillary block risk |
| Increased lens thickness with age | Forward iris displacement |
| Altered aqueous outflow | Sudden IOP rise in acute attacks |
| Vascular factors | Optic nerve perfusion risk |
| Biomechanics | IOP fluctuations and optic nerve stress |
PACG commonly affects older adults, hyperopes, and those with short axial length, thicker crystalline lenses, shallow anterior chambers, or a positive family history.
Clinical Insight for Eye-Care Practitioners
Early recognition prevents irreversible optic nerve damage. Key assessments include:
- Gonioscopy
- Anterior chamber depth estimation
- IOP measurement
- AS-OCT and UBM when available
- Family history and refractive status review
Early prophylactic laser peripheral iridotomy (LPI) is often recommended in anatomically narrow angles to relieve pupillary block.
Final Note
Primary angle-closure glaucoma remains a significant cause of avoidable blindness worldwide. Understanding anatomical predisposition and ocular fluid dynamics equips clinicians to identify at-risk eyes early and implement preventive care.
Credit: ResearchGate (Diagram Source)
