Interpreting visual field test results can often feel overwhelming, especially when faced with complex patterns and subtle losses. But with a systematic approach, it becomes much easier to identify the location and cause of the defect. Rather than jumping straight to a global assessment, it’s important to evaluate the results step by step.
Here’s a five-step framework to help you interpret visual fields with precision and confidence.
1. Start by Determining: Normal or Abnormal?
Begin with a simple question: is the field normal or abnormal? Review each eye individually. Automated perimetry makes this easier by comparing the patient’s results to age-matched normative data—both on a point-by-point basis and through summary indices.
If both eyes show normal findings clinically and statistically, no further workup may be needed.
2. Evaluate Testing Reliability and Artifacts
If you detect abnormalities, your next step is to ensure the results are trustworthy. Check for:
- Proper near correction
- Adequate pupil size
- Steady fixation throughout the test
Also rule out artifacts caused by external factors like:
- Lens rim shadows
- Drooping eyelids (ptosis)
- Patient fatigue or drowsiness
Artifacts can easily mimic true pathology. When in doubt, consult the technician who administered the test to better understand the patient’s condition and cooperation.
3. Is the Defect in One Eye or Both?
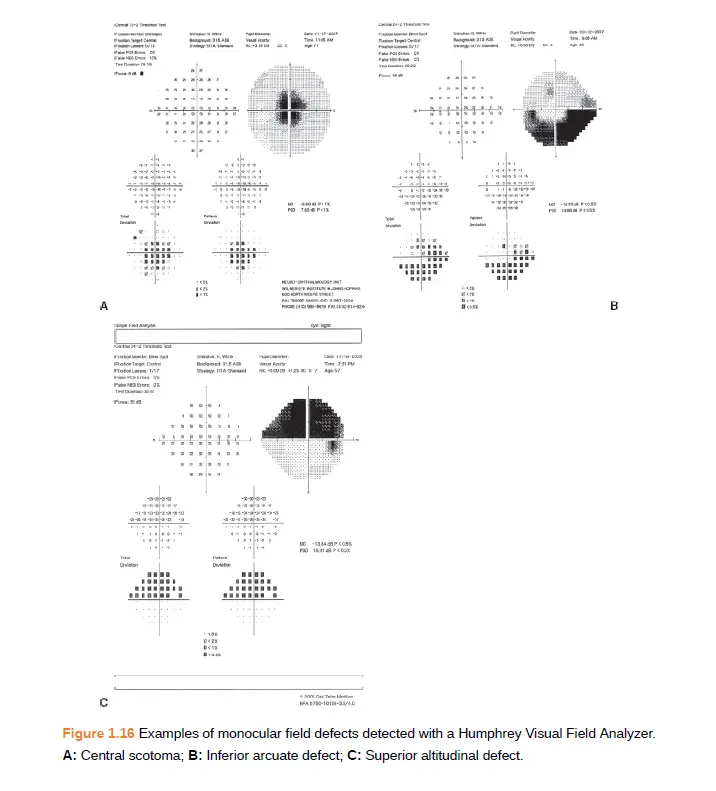
This is a crucial step for localizing the lesion. Determine if the defect is monocular (one eye) or binocular (both eyes):
- Monocular defects point to issues before the optic chiasm, such as optic nerve or retinal disorders.
- Binocular defects suggest lesions at or beyond the chiasm, such as strokes, tumors, or bilateral nerve damage.
4. Localize the Defect Based on Field Pattern
Look closely at which part of the field is affected—superior, inferior, nasal, temporal, or central. The defect’s location provides critical clues:
- Bitemporal hemianopia: Often indicates chiasmal compression (e.g., pituitary tumors).
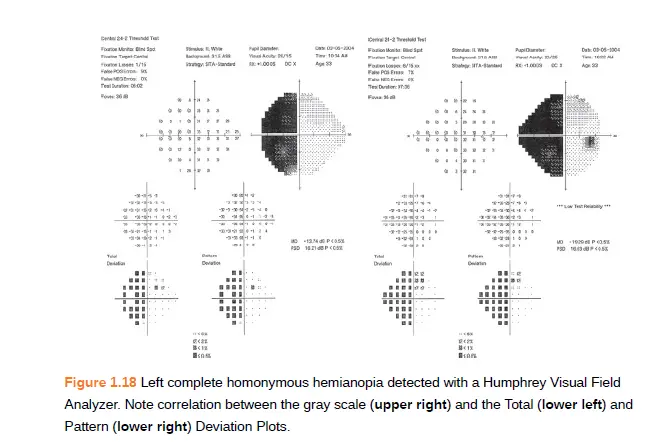
- Homonymous hemianopia: A nasal field loss in one eye with a temporal loss in the other points to a retrochiasmal lesion.
- Binasal defects: May indicate glaucoma or bilateral optic nerve pathology.
- Central scotomas: Often related to macular disease or toxic/nutritional optic neuropathies.
5. Analyze the Shape and Characteristics of the Defect
This final step brings all the details together. Ask yourself:
- Does the defect respect the vertical or horizontal meridian?
- Is it arcuate, round, pie-shaped, or irregular?
- In binocular field loss, is it congruous (symmetrical) or incongruous (asymmetrical)?
- Are the edges sharp or fuzzy?
Patterns matter. For example, arcuate defects are common in glaucoma, while congruent homonymous hemianopias are often seen in occipital lobe strokes.
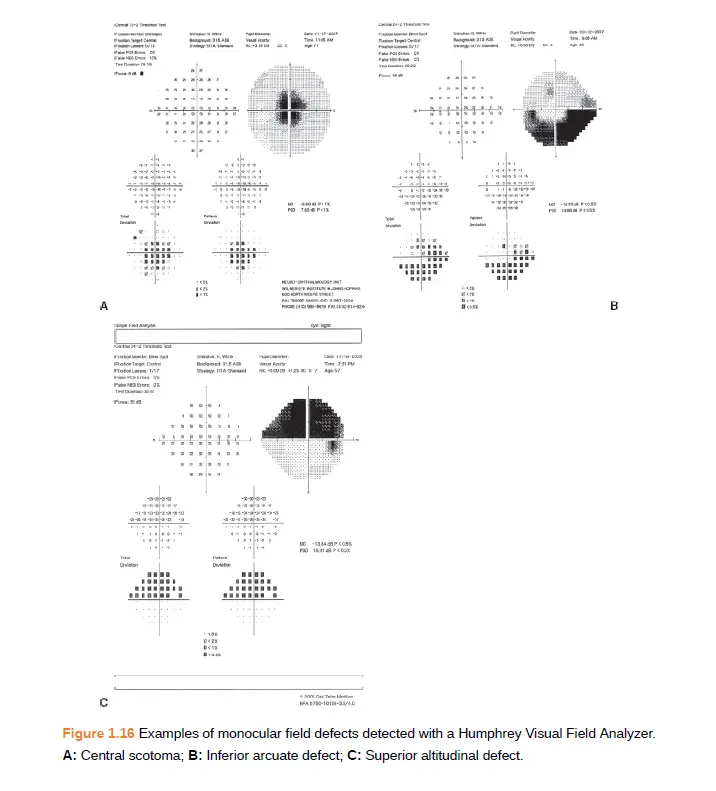
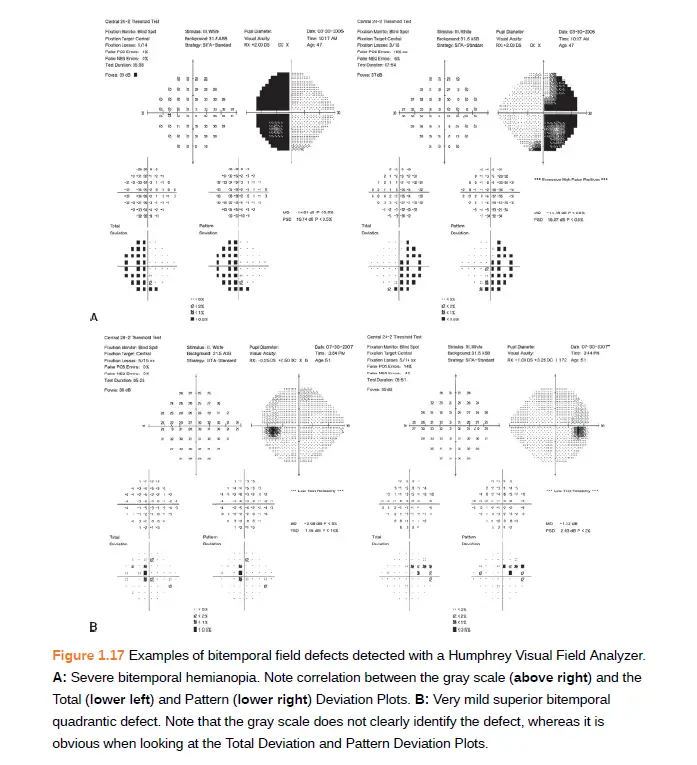
Images taken from book- Walshs and Hoyts clinical neuropthalmology (get from Amazon)