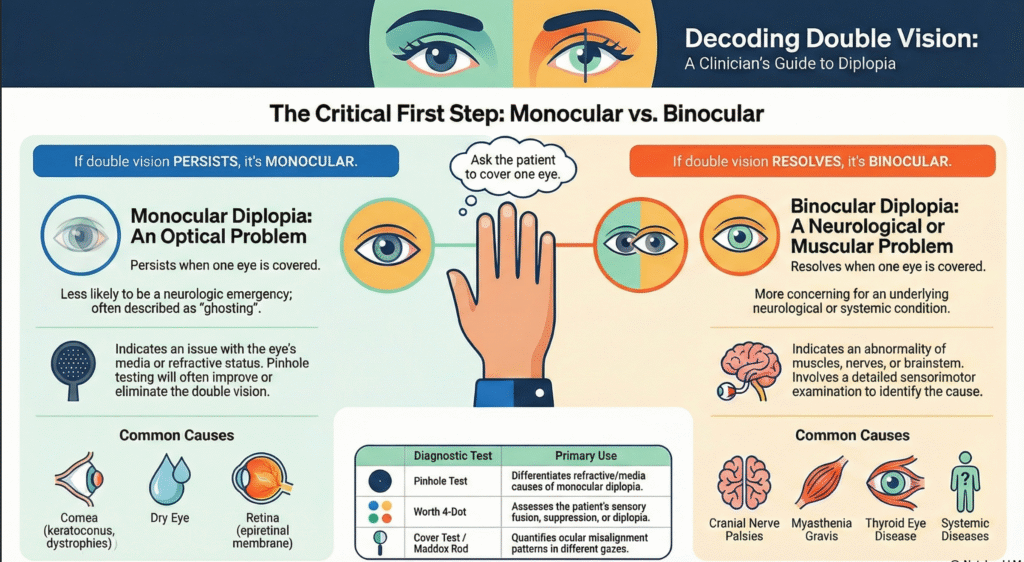
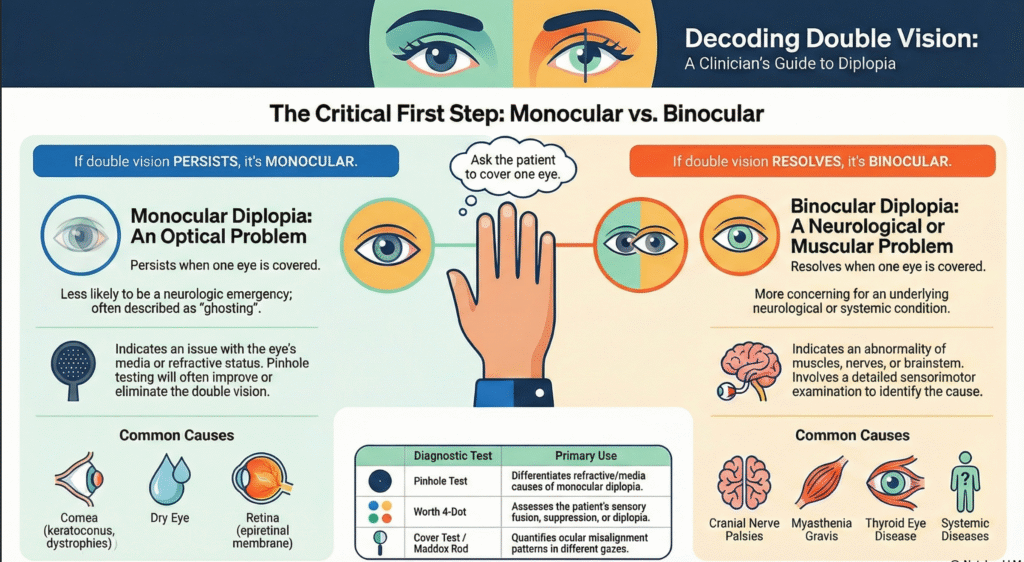
Monocular vs Binocular Diplopia: A Step-by-Step Clinical Guide to Double Vision
Double vision, or diplopia, is a symptom that often alarms patients and clinicians alike. While it can sometimes indicate a serious neurological condition, many cases arise from benign optical causes. The most critical and time-saving step in evaluating diplopia is a simple one: determining whether the double vision is monocular or binocular.
This distinction immediately narrows the differential diagnosis and guides appropriate management.
The First and Most Important Question in Diplopia
Ask the patient to cover one eye.
- If double vision persists → the diplopia is monocular
- If double vision resolves → the diplopia is binocular
This single step separates optical problems from ocular misalignment or neurological causes.
Monocular Diplopia: An Optical Problem
Key Clinical Features
- Persists when one eye is covered
- Usually described as ghosting, shadowing, or overlapping images
- Less likely to represent a neurological emergency
- Typically improves with pinhole testing
Monocular diplopia originates from within the eye itself, rather than from misalignment between the two eyes.
Common Causes of Monocular Diplopia
- Corneal Abnormalities
- Keratoconus
- Corneal dystrophies
- Irregular astigmatism
- Tear Film Issues
- Dry eye disease
- Tear film instability
- Lens Abnormalities
- Early or irregular cataract
- Retinal Causes
- Epiretinal membrane
- Macular pathology
Diagnostic Clues
- Pinhole test improves vision → refractive or media cause likely
- Refraction reveals irregular astigmatism
- Slit-lamp examination identifies corneal or lens pathology
Monocular diplopia is managed by addressing the underlying ocular cause, not by neurological evaluation.
Binocular Diplopia: A Neurological or Muscular Concern
Key Clinical Features
- Resolves when either eye is covered
- Caused by misalignment of the visual axes
- Requires careful evaluation for neuromuscular or systemic disease
- Often associated with gaze-dependent symptoms
Binocular diplopia arises when the brain receives two non-corresponding images due to eye misalignment.
Common Causes of Binocular Diplopia
- Cranial Nerve Palsies
- Third, fourth, or sixth nerve involvement
- Neuromuscular Disorders
- Myasthenia gravis
- Orbital Disease
- Thyroid eye disease
- Systemic or Neurological Conditions
- Diabetes
- Hypertension
- Brainstem pathology
Why Binocular Diplopia Is More Concerning
Binocular diplopia may signal:
- Acute neurological disease
- Progressive muscle weakness
- Brainstem involvement
Prompt recognition is essential, especially in sudden-onset diplopia, diplopia with headache, ptosis, or pupillary involvement.
Key Diagnostic Tests in Diplopia Evaluation
Pinhole Test
- Differentiates refractive or media causes
- Primarily useful in monocular diplopia
Worth 4-Dot Test
- Assesses sensory fusion
- Detects suppression or diplopia
Cover Test and Maddox Rod
- Quantifies ocular deviation
- Identifies patterns of misalignment in different gazes
A structured sensorimotor examination is essential in binocular diplopia cases.
Clinical Takeaway for Practitioners
- Always start by covering one eye
- Monocular diplopia points to optical causes
- Binocular diplopia suggests muscle, nerve, or neurological involvement
- Early differentiation prevents unnecessary investigations and delays in care
This simple approach allows clinicians to triage diplopia efficiently, ensuring timely referral when needed and focused treatment when the cause is ocular.
