Filamentary Keratitis Notes

Optometry Notes: Filamentary Keratitis
Definition:
Filamentary keratitis is a chronic ocular surface disorder characterized by the presence of filaments on the corneal epithelium. These filaments consist of degenerated epithelial cells, mucus, and inflammatory debris, and are typically adherent to the corneal surface.
Etiology and Associations
Filamentary keratitis is not a primary condition but a secondary manifestation associated with:
- Dry eye disease (aqueous-deficient or evaporative)
- Superior limbic keratoconjunctivitis (SLK)
- Neurotrophic keratitis
- Post-surgical ocular surface changes (e.g., LASIK, cataract surgery)
- Recurrent corneal erosions
- Systemic autoimmune conditions such as:
- Sjögren’s syndrome
- Rheumatoid arthritis
- Lid margin disease, including Demodex infestation
- Long-term contact lens wear
Pathophysiology
- Filaments form due to poor epithelial adherence and mucin imbalance.
- They typically attach at areas of epithelial damage and are pulled during blinking, causing further trauma and a self-perpetuating cycle.
- Tear film instability and chronic inflammation play key roles.
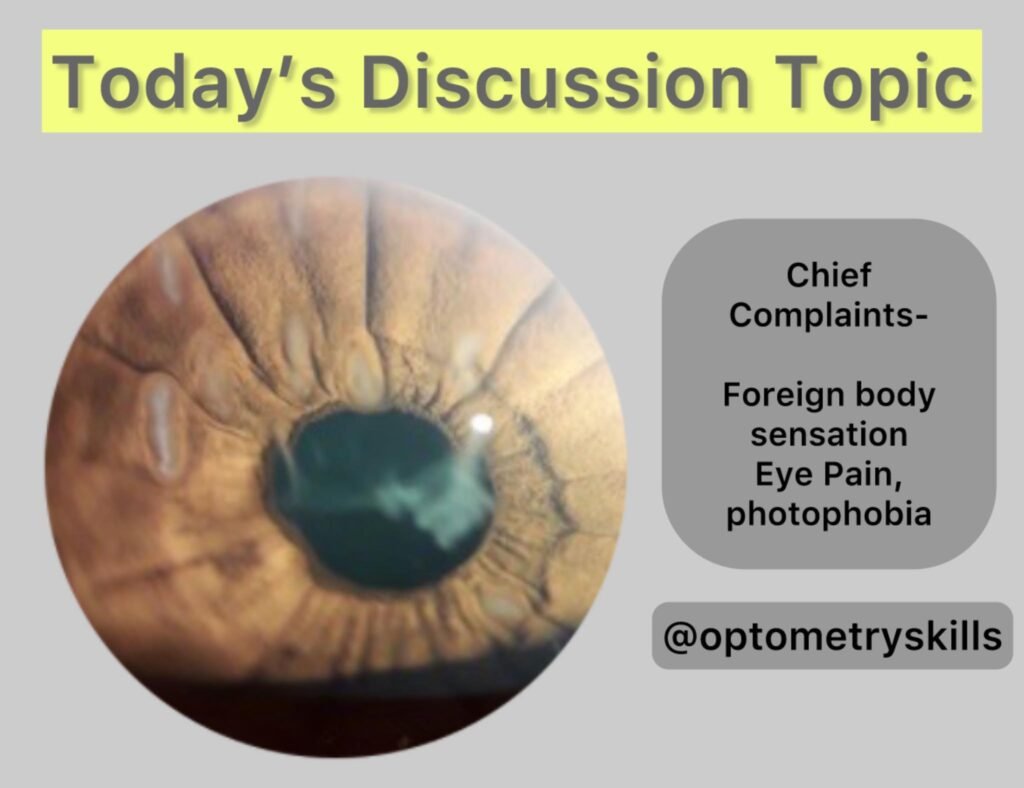
Symptoms
Patients may report:
- Foreign body sensation
- Photophobia
- Ocular discomfort or pain
- Lacrimation (reflex tearing)
- Intermittent blurred vision
- Blepharospasm in severe cases
Symptoms are often disproportionate to the visible pathology.
Clinical Signs
- Filaments: Small, gray-white, mucus-like strands on the corneal surface.
- Composed of degenerated epithelial cells embedded in mucus.
- Usually visible with slit-lamp examination and may stain with fluorescein, rose bengal, or lissamine green.
- Filaments often have one end adherent to the cornea and may be mobile.
- Additional findings:
- Punctate epithelial erosions
- Conjunctival hyperemia
- Reduced tear break-up time (TBUT)
- Evidence of underlying ocular surface disease
Diagnostic Considerations for Optometrists
- Slit-lamp biomicroscopy is key to diagnosis.
- Staining techniques help identify the extent of ocular surface damage and filament attachment.
- Consider the broader ocular and systemic context—evaluate for dry eye, meibomian gland dysfunction, or systemic autoimmune diseases.
- Always explore patient history, especially:
- Contact lens use
- Past ocular surgery
- Chronic topical drop use
- Dryness or systemic symptoms suggestive of autoimmune disease
Course and Prognosis
- Filamentary keratitis can be chronic and relapsing.
- Symptoms tend to persist until underlying factors (e.g., tear instability, lid disease) are addressed.
- Visual acuity is often preserved but can be intermittently reduced due to filaments or associated surface irregularity.
Treatment Strategy
A targeted, stepwise approach is essential:
- Mechanical Removal
- Remove filaments under topical anesthesia using fine forceps; grip at the base to reduce recurrence
- Address Tear Film and Ocular Surface
- Use preservative-free artificial tears (e.g., Systane, TheraTears) frequently
- Apply punctal occlusion for aqueous-deficient cases
- Mucolytics & Hypertonic Agents
- Topical N‑acetylcysteine 10% TID–QID (compounded) can dissolve mucus
- Hypertonic saline (2% solution, 5% ointment) helps reduce corneal edema
- Anti-inflammatory Treatment
- Short-term corticosteroids (e.g., loteprednol, fluorometholone) or NSAIDs (e.g., cyclosporine A, lifitegrast) control surface inflammation
- Address systemic inflammation (e.g., Sjögren’s) and collaborate with rheumatology if needed
- Advanced Therapies for Refractory Cases
- Bandage or scleral contact lenses to protect epithelium
- Amniotic membrane grafts (e.g., PROKERA®) promote healing
- Botulinum toxin injections for filaments refractory to other treatments
- Autologous serum drops for severe cases
Follow-Up & Prognosis
- FK often requires continuous management; recurrence is common without treating root causes
- Follow-up every 3–4 months for ocular surface control is advisable in chronic cases
- Collaborate with systemic care providers when autoimmune or infectious factors are present
Conclusion
Filamentary keratitis is a multifactorial condition requiring careful identification of underlying causes and a comprehensive treatment plan. For optometrists, combining mechanical removal with a regime that includes lubrication, inflammation control, mucolytics, and advanced therapies when needed can lead to effective symptom resolution and reduce recurrence. Collaborative care with specialists enhances outcomes for systemic or ocular comorbidities.
Reference you can study- Optometry Times and Review of Optometry
