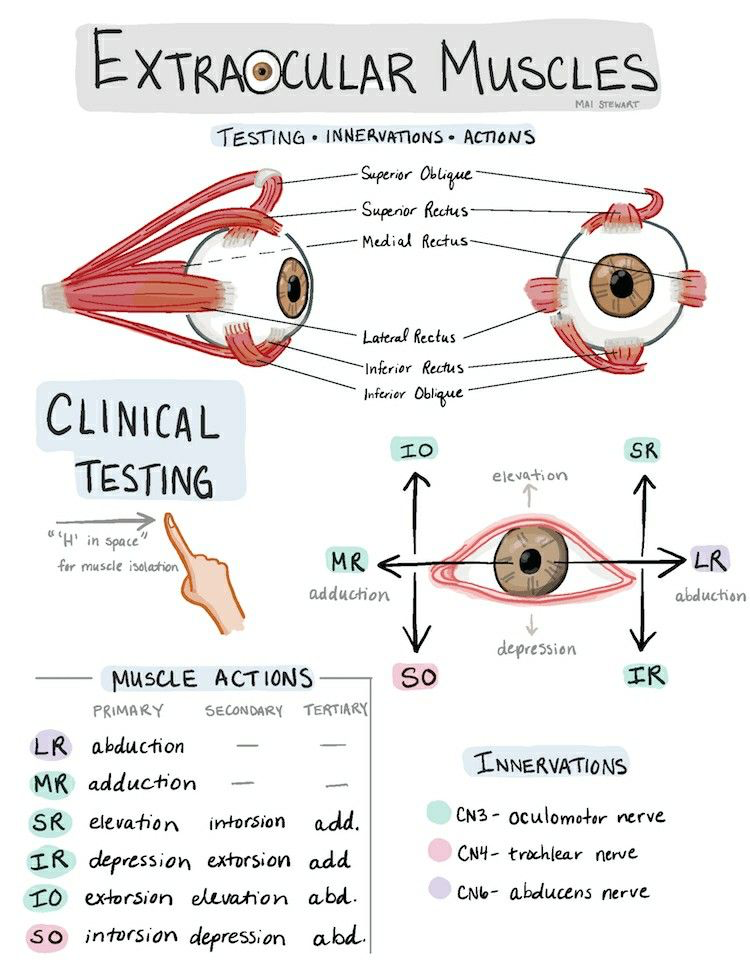
Read about clinical tips for writing accurate prescriptions based on extraocular muscle function, including actions, innervations, and testing methods for the superior, inferior, medial, and lateral eye muscles to identify nerve involvement and manage diplopia effectively.

Clinical Tips for Prescribing Based on Extraocular Muscle Function
1. Understand the Muscle Functions
- Superior Rectus (SR): Elevates eye, intorsion, adduction.
- Test: Ask patient to look up and slightly inward (“H” pattern).
- Innervation: CN III (oculomotor)
- Inferior Rectus (IR): Depresses eye, extorsion, adduction.
- Test: Look down and slightly inward.
- Innervation: CN III
- Medial Rectus (MR): Adduction (moves eye toward nose).
- Test: Ask patient to look medially.
- Innervation: CN III
- Lateral Rectus (LR): Abduction (moves eye outward).
- Test: Ask patient to look laterally.
- Innervation: CN VI (abducens)
- Superior Oblique (SO): Intorsion, depression, abduction.
- Test: Look down and out.
- Innervation: CN IV (trochlear)
- Inferior Oblique (IO): Extorsion, elevation, abduction.
- Test: Look up and out.
- Innervation: CN III
2. Use the “H Pattern” for Muscle Isolation
- This is the standard technique for clinical EOM testing.
- Move the patient’s gaze in an H-shaped pattern to isolate vertical, horizontal, and oblique muscles.
- Tip: Always test both eyes individually to identify subtle weaknesses or restrictions.
3. Check for Primary, Secondary, and Tertiary Actions
- Example: Superior Rectus
- Primary: Elevation
- Secondary: Intorsion
- Tertiary: Adduction
- Understanding these allows you to detect muscle palsies or nerve involvement that may not be apparent in a straight gaze.
4. Note the Innervation
- CN III (Oculomotor) → SR, IR, MR, IO
- CN IV (Trochlear) → SO
- CN VI (Abducens) → LR
- Clinical tip: If a single nerve is affected, multiple muscles may show dysfunction. For example:
- CN IV palsy → SO weakness → vertical diplopia when looking down/out.
- CN VI palsy → LR weakness → horizontal diplopia on lateral gaze.
5. Prescription Considerations
- Document which muscles are weak and corresponding direction of gaze limitation.
- Include degree of deviation (e.g., prism diopters) if prescribing for strabismus or diplopia.
- Consider compensatory head posture (chin up/down, head tilt) in the prescription notes.
- For occlusion or prism therapy, target the direction corresponding to the weak muscle’s primary action.
- Always correlate with patient symptoms (double vision, eye strain, asthenopia).
Nb: Image credit in Pic
